Venous Thrombosis
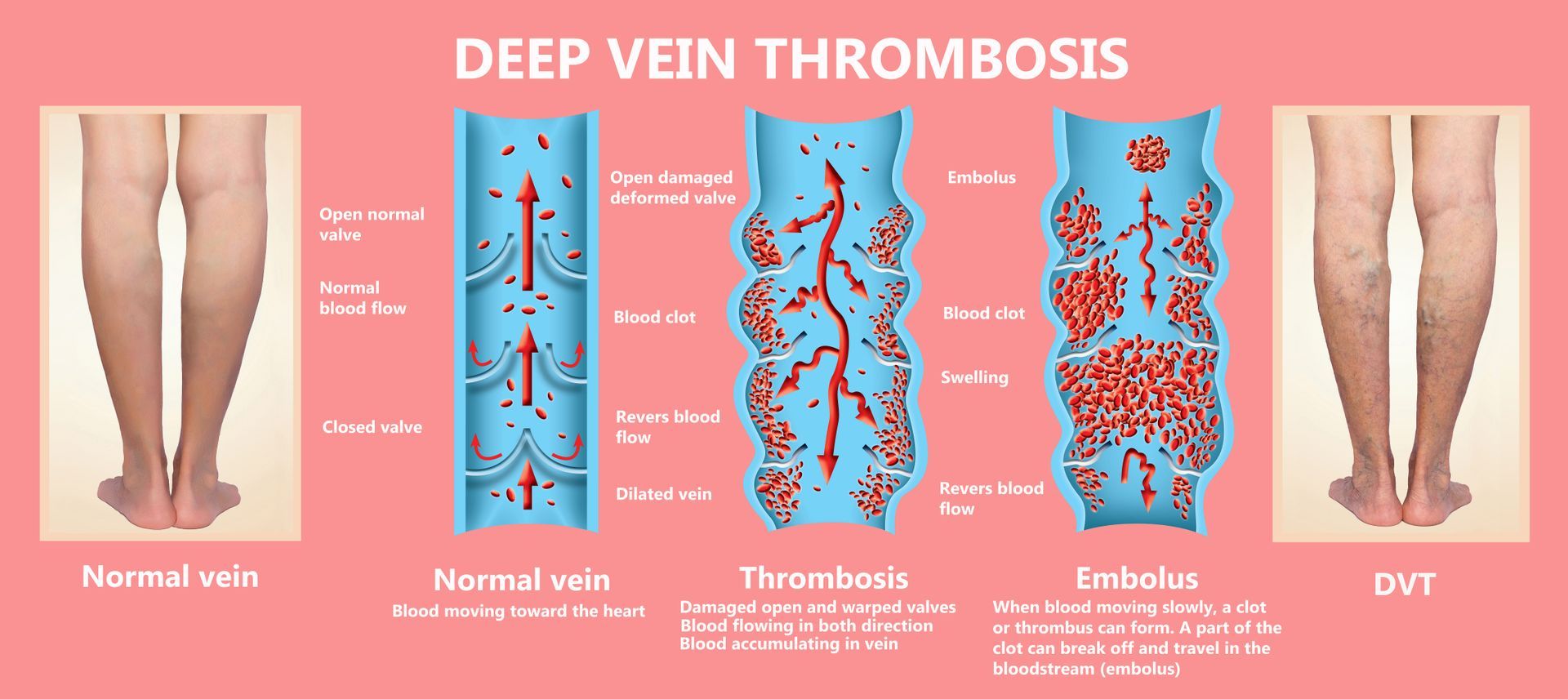
Blood clots are part of our bodies’ normal healing process. However, clots can be harmful if they become stuck in large veins. This complication is known as venous thrombosis (or vein thrombosis). When a blood clot becomes stuck in a large, deep vein, deep vein thrombosis (DVT) is diagnosed.
Studies show that around 1 in every 1,000 Americans will develop DVT at some point in their lives. If left untreated, DVT can become a serious condition that leads to other health complications. It is important to receive diagnosis and treatment quickly and accurately.
What Is Venous Thrombosis?
Doctors use several different terms to talk about blood clots — familiarizing yourself with them can help you better understand your condition. The medical term for a blood clot is a thrombus. A venous thromboembolism (VTE) occurs when a blood clot blocks blood flow in one of your veins. VTE can be broken down into two main types — DVT and pulmonary embolism (PE).
DVT mainly affects the large veins in the lower leg, thigh, and pelvis. These veins are responsible for bringing oxygen-depleted blood from your lower body back up to your heart and lungs. DVT can also develop in your arms, particularly if you have had an intravenous (IV) central line or catheter placed to deliver medications or take blood samples. DVT is the most common type of VTE.
PE typically develops as a complication of DVT. This occurs when a blood clot breaks off and travels through your bloodstream back toward your heart. As blood flows through your lungs, the clot can become stuck. This increases the blood pressure within your lungs — as a result, your heart has to work harder to pump blood against the pressure. If left untreated, PE can eventually result in right-heart failure.
While DVT and PE affect the deep veins in your body, blood clots can also develop in the veins near the surface of your skin (superficial veins). This leads to a condition known as superficial thrombophlebitis, or superficial venous thrombosis (SVT). SVT typically affects the legs and may be a sign of DVT or another underlying vein issue.
What Causes Venous Thrombosis?
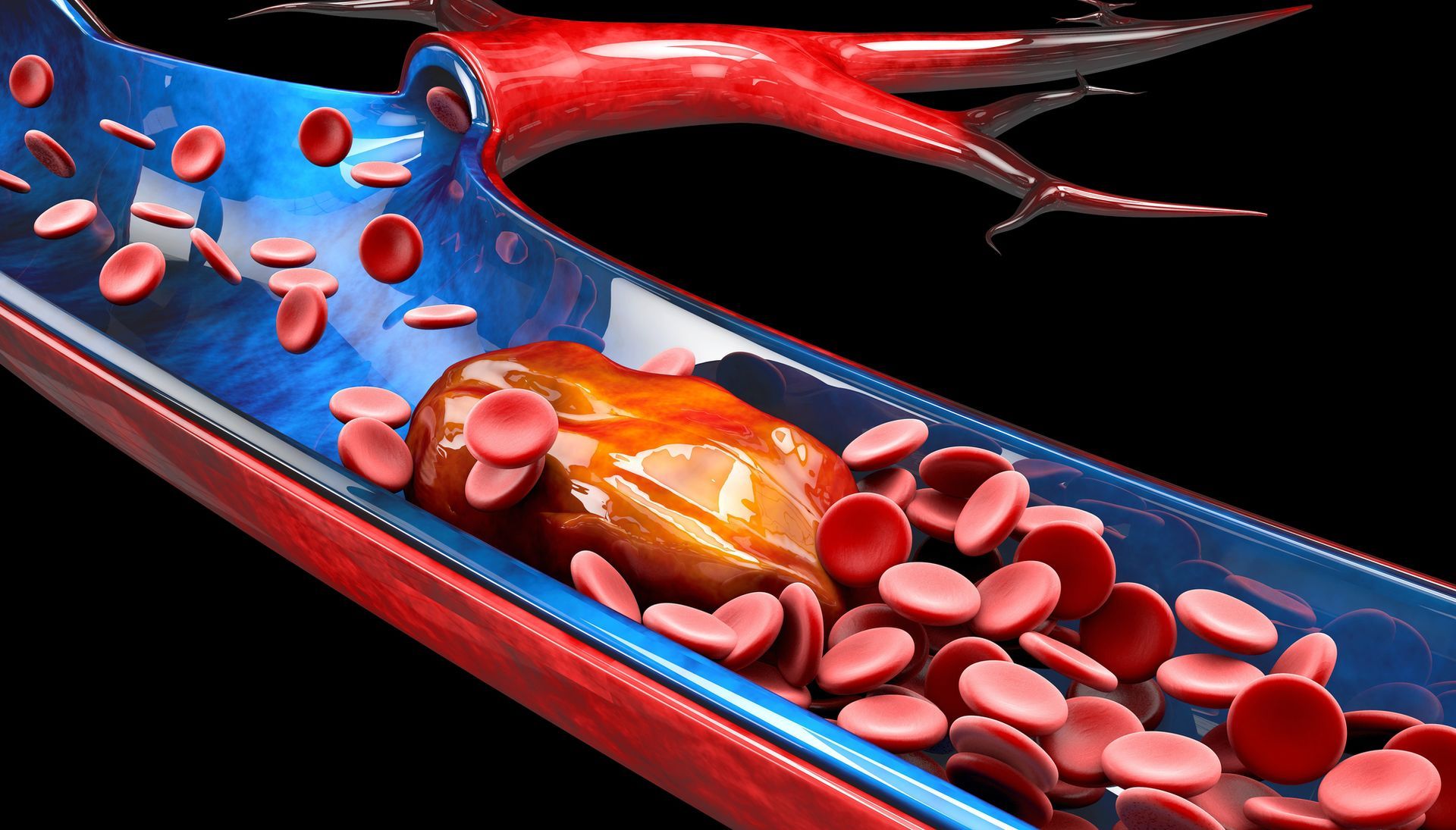
Your body makes blood clots to heal damaged blood vessels. When damage occurs, your spleen begins making specialized cell fragments known as platelets. These fragments travel to the damaged blood vessel, sticking to it to create a plug to stop bleeding. Other specialized proteins known as clotting factors come together to form a mesh that recruits red blood cells to cover the platelet plug. Together, these cells and proteins make a blood clot.
Sometimes, blood clots form outside of blood vessel injuries, putting you at a higher risk of venous thrombosis and other complications. This is more common when blood flow to the legs is slowed, which can occur if you’ve been sitting for a long time. Many people understand that blood clots are common after bedrest, surgery, or sitting for too long in a car or airplane. They may also form after an infection or other injury.
There are several other risk factors that increase the chances of developing a blood clot and DVT. These include:
- Personal history of blood clots or DVT
- Family history of blood clots or DVT
- Older age
- Varicose veins
- Taking hormonal birth control pills or hormone replacement therapy for menopause
- Pregnancy or having recently delivered a baby
- Vein injuries caused by bone fractures or severe muscle injuries
- Being overweight or having obesity
- Certain autoimmune diseases such as vasculitis (inflammation of the blood vessels), lupus, or inflammatory bowel disease
- Certain blood clotting disorders, such as factor V Leiden, which lead to an excess of blood clots
- Smoking tobacco
- Having certain types of cancer
- Chemotherapy treatment
How Do You Know If You Have Venous Thrombosis?
According to the Cleveland Clinic, nearly 30 percent of people with DVT do not show any symptoms. Others may have mild symptoms that may not raise any concern. If you begin to notice any of the following symptoms, contact your doctor right away. Early treatment for venous thrombosis can limit other health complications later on.
Venous thrombosis symptoms can vary depending on which vein is affected. With DVT, you may notice:
- Redness, warmth, and/or swelling in one leg
- Enlarged veins (known as cords)
- Pelvic discomfort
- Pain when walking or bending your leg at the knee
- Muscle pain and cramping that comes and goes
DVT can also develop in the deep veins in your abdomen that bring blood from the intestines back to your heart. If you develop a blood clot in one of these veins, you may experience severe stomach pain, nausea, or vomiting.
PE symptoms that may occur alongside DVT symptoms include:
- Sharp chest pain that feels similar to a heart attack
- Shortness of breath and wheezing
- Clammy or pale skin
- Excessive sweating
- Rapid heartbeat
- Dizziness, which may cause you to pass out
- Coughing up mucus with or without blood
How Is Venous Thrombosis Diagnosed?
If your doctor thinks you may have DVT, they will order some tests to confirm a diagnosis. These include blood tests to check for specific proteins and imaging tests to look for blood clots in a suspected area.
One blood test used to diagnose venous thrombosis is a D-dimer test. D-dimer is a protein fragment that is made when a blood clot dissolves. Normally, you should have low D-dimer levels — if they are high, they may point to a blood clot. This one test cannot confirm a DVT diagnosis alone, so your doctor will use other tests as well.
Your doctor will use ultrasound to visualize your veins and look for a blood clot. This technique uses a special instrument known as a transducer to send sound waves into your body. These waves bounce off your veins and other internal structures and are detected by the transducer to form images. There are a few different ultrasound techniques that vein doctors use, including Doppler ultrasound, duplex ultrasound, and compression ultrasound.
Doppler ultrasound provides audio so your doctor can hear how well blood is flowing through your veins. This is typically used alongside duplex ultrasound to visualize blood flow and look for clots. A compression ultrasound may be used to look for blood clots specifically in the legs. The doctor will apply pressure with the transducer to check if your veins compress normally or are stiff from blood clots.
Treatments for Venous Thrombosis
Venous thrombosis can be treated with medications and minimally invasive procedures to help remove blood clots and prevent them from forming again. The most common first-line treatment is prescribing a blood thinner (oral anticoagulant). These medications help “thin” your blood by interfering with clotting factors. Some medications help prevent your body from making more clotting factors, while others directly interfere with their function.
Blood Thinners
There are a few different types of anticoagulants that your doctor may prescribe to treat DVT. These include warfarin and direct oral anticoagulants (DOACs).
Warfarin
Warfarin (sold under the brand names Coumadin and Jantoven) has been used for several years as the mainstay treatment for blood clots. Your liver makes clotting factors with a specialized enzyme that uses vitamin K. Warfarin blocks this enzyme’s ability to use vitamin K, reducing your clotting factor levels. As a result, your blood can’t form blood clots as easily.
While warfarin is known to be an extremely effective blood thinner, it does have some qualities that may make it difficult for some people to take. You will need monthly bloodwork to monitor your blood’s ability to clot — sometimes, warfarin thins the blood too much, increasing your risk of accidental bleeding. Other side effects of warfarin include gas or bloating, abdominal pain, changes in taste, and hair loss.
Since warfarin competes with vitamin K in your body, it is important to limit your consumption of foods rich in it. These foods may make warfarin less effective, increasing the risk of blood clots. Vitamin K can be found in:
- Dark, leafy green vegetables like kale, spinach, swiss chard, mustard greens, collard greens, and turnip greens
- Other dark green vegetables like broccoli, brussels sprouts, and asparagus
- Seaweed
- Chamomile or green teas
- Cranberry and grapefruit juice
Direct Oral Anticoagulants
DOACs are a newer class of medications that have been found to be as safe and effective as warfarin while requiring less monitoring. Depending on your case of venous thrombosis, your doctor may prescribe you a DOAC instead of warfarin.
There are two main types of DOACs that block either clotting factors or the protein thrombin, both of which are involved in the blood clotting process. There are several different DOACs approved for treating and preventing blood clots, including:
- Dabigatran (Pradaxa): direct thrombin inhibitor
- Apixaban (Eliquis): factor Xa inhibitor
- Rivaroxaban (Xarelto): factor Xa inhibitor
- Betrixaban (Bevyxxa): factor Xa inhibitor
- Edoxaban (Savaysa): factor Xa inhibitor
When taking a DOAC, it is important to take it at the same time every day for it to be effective. Common side effects of these medications include heartburn, abdominal pain, nausea, dizziness, muscle spasms, and skin rashes.
DVT Thrombolysis
DVT thrombolysis is a minimally invasive surgical technique used in emergencies to treat DVT by removing or clearing away large blood clots. During this procedure, a specially trained vein doctor uses ultrasound to guide a long, thin, flexible tube known as a catheter into the vein that contains the blood clot. In some cases, the doctor may use a contrast dye to better visualize the veins.
Once the catheter is inserted near the clot, the doctor administers clot-dissolving medications or a saline (salt water) solution to break up the clot. Some catheters use a tool to remove the blood clot — this procedure is known as a thrombectomy. Catheter-based treatments require only a small incision in the skin, reducing recovery times and leaving little scarring.
Inferior Vena Cava Filter
If you are unable to take blood thinners or they are not effective in preventing blood clots, your doctor may recommend an inferior vena cava (IVC) filter. The IVC is the largest vein in your body that brings blood from the lower half of your body back to the lungs and heart.
A surgical procedure can be performed to place an IVC filter in this vein, which filters the blood to prevent clots from traveling from your legs into your lungs. This is an effective method for preventing PE — however, it does not prevent the formation of new blood clots in other areas of your body.
To place an IVC filter, vein specialist will numb an area around your groin or neck and make a small incision for inserting a catheter. This catheter contains the collapsed IVC filter, which is gently maneuvered into your IVC. Once there, vein specialist will push the filter out, allowing it to expand in the vein. The catheter is removed and the filter remains in place.
Preventing Venous Thrombosis
If you are at a higher risk of developing a blood clot, there are steps you can take to help prevent them. The Centers for Disease Control and Prevention (CDC) recommends exercising when sitting for extended periods of time and wearing compression stockings.
Exercise
Exercise keeps blood moving throughout your body, which can lower your risk of blood clots. If you are planning on sitting for long periods of time, try to get up and walk every one to two hours. You can also do sitting exercises to move your feet and legs to promote blood flow. The CDC recommends:
- Flexing and relaxing your leg muscles, including your calves and thighs
- Raising and lowering your toes while keeping your heels flat on the floor
- Raising and lowering your heels while keeping your toes flat on the floor
Compression Stockings
Venous thrombosis in the legs can develop from slow blood flow through the feet and legs. To help combat this, doctors recommend wearing compression stockings to promote blood flow from the lower half of the body back to the lungs and heart. These stockings are specially designed with a pressure gradient that puts the most amount of pressure on the feet and ankles and gradually decreases as they go upward.
Compression stockings help reduce swelling associated with DVT. They can also be worn on long airplane trips and car rides to prevent DVT from occurring. These socks can be purchased at a local pharmacy or online. Before ordering, be sure to measure your legs to order the correct size.
Complications from Venous Thrombosis
One of the most common complications of DVT is post-thrombotic syndrome (PTS). This condition affects up to half of people who have recovered from DVT. When a blood clot becomes stuck in a vein, it blocks blood flow, leading to a buildup of pressure. This damages the vein, causing blood to leak and pool around it. This is most common in people who have DVT in their leg, which causes blood to pool at the ankles.
Signs of PTS after a blood clot include:
- Leg cramping or heaviness
- Leg tingling or itching
- Pain, redness, and/or swelling in the leg that gets better with rest and elevation
- Leg ulcers (open sores)
If you notice any of these signs after recovering from DVT, talk to your doctor. They will prescribe compression stockings with a higher pressure grade to help move pooled blood away from your feet and ankles. They will also prescribe medication to treat ulcers or sores.
Frequently Asked Questions (FAQ)

DR. AMIT POONIA M.D.
Your New Jersey Vein Specialist
Dr. Poonia is double board-certified in interventional pain management and anesthesiology.
Dr. Poonia’s philosophy is based on teamwork, cooperation, and collaboration among his patients’ treatment teams. He believes that healthcare providers work
best when they work together to accurately diagnose a patient’s problem, find effective treatments, and provide maximum rehabilitation and quality of life improvements.
Dr. Poonia customizes his treatment plans based on each patient’s unique characteristics. He employs the latest minimally-invasive technologies to enhance comfort during treatment and to speed recovery.
References
- Blood Clots. Cleveland Clinic. September 24, 2020. Accessed January 15, 2023. https://my.clevelandclinic.org/health/diseases/17675-blood-clots.
- Cushman M. Epidemiology and risk factors for venous thrombosis. Semin Hematol. 2007;44(2):62-69. doi:10.1053/j.seminhematol.2007.02.004
- Deep Vein Thrombosis (DVT). Cleveland Clinic. March 28, 2022. Accessed January 15, 2023.https://my.clevelandclinic.org/health/diseases/16911-deep-vein-thrombosis-dvt.
- Fiumara K, Goldhaber SZ. Cardiology patient pages. A patient’s guide to taking coumadin/warfarin. Circulation. 2009;119(8):e220-2. doi:10.1161/CIRCULATIONAHA.108.803957
- How Does Blood Clot? National Heart, Lung, and Blood Institute. March 24, 2022. Accessed January 14, 2023. https://www.nhlbi.nih.gov/health/clotting-disorders/how-blood-clots.
- Huisman MV, Klok FA. Diagnostic management of acute deep vein thrombosis and pulmonary embolism. J Thromb Haemost. 2013;11(3):412-22. doi:10.1111/jth.12124
- Kelkar AH, Rajasekhar A. Inferior vena cava filters: a framework for evidence-based use. Hematology Am Soc Hematol Educ Program. 2020;2020(1):619-628. doi:10.1182/hematology.2020000149
- Kim KA, Choi SY, Kim R. Endovascular treatment for lower extremity deep vein thrombosis: An overview. Korean J Radiol. 2021;22(6):931-943. doi:10.3348/kjr.2020.0675
- Lim CS, Davies AH. Graduated compression stockings. CMAJ. 2014;186(10):E391-E398. doi:10.1503/cmaj.131281
- Marchiori A, Mosena L, Prandoni P. Superficial vein thrombosis: Risk factors, diagnosis, and treatment. Semin Thromb Hemost. 2006l32(7):737-43. doi:10.1055/s-2006-951459
- Pulivarthi S, Gurram MK. Effectiveness of D-dimer as a screening test for venous thromboembolism: An update. N Am J Med Sci. 2014;6(10):491-499. doi:10.4103/1947-2714.143278
- Pulmonary Embolism. National Heart, Lung, and Blood Institute. September 19, 2022. Accessed January 15, 2023. https://www.nhlbi.nih.gov/health/pulmonary-embolism.
- Sachdeva A, Dalton M, Lees T. Graduated compression stockings for prevention of deep vein thrombosis. Cochrane Database Syst Rev. 2018;2018(11):CD001484. doi:10.1002/14651858.CD001484.pub4
- Scarvelis D, Wells PS. Diagnosis and treatment of deep-vein thrombosis. CMAJ. 2006;175(9):1087-1092. doi:10.1503/cmaj.060366
- Stone J, Hangge P, Albadawi H, et al. Deep vein thrombosis: Pathogenesis, diagnosis, and medical management. Cardiovasc Diagn Ther. 2017;7(Suppl 3):S276-S284. doi:10.21037/cdt.2017.09.01
- Streiff MB, Agnelli G, Connors JM, et al. Guidance for the treatment of deep vein thrombosis and pulmonary embolism. J Thromb Thrombolysis. 2016;41:32-67. doi:10.1007/s11239-015-1317-0
- Vazquez SR, Khan SR. Postthrombotic syndrome. Cardiology patient page. Circulation. 2010;121(8):e217-9. doi:10.1161/CIRCULATIONAHA.109.925651
- Vena Cava Filters. Cleveland Clinic. March 24, 2022. Accessed January 15, 2023. https://my.clevelandclinic.org/health/treatments/17609-vena-cava-filters.
- Wadhera RK, Russell CE, Piazza G. Cardiology patient page. Warfarin versus novel oral anticoagulants: how to choose? Circulation. 2014;130(22):e191-3. doi:10.1161/CIRCULATIONAHA.114.010426
- What are Direct-Acting Oral Anticoagulants (DOACs)? American Heart Association. Accessed January 15, 2023. https://www.heart.org/-/media/files/health-topics/answers-by-heart/what-are-doacs.pdf.
- What is Venous Thromboembolism? Centers for Disease Control and Prevention. June 9, 2022. Accessed January 15, 2023.
https://www.cdc.gov/ncbddd/dvt/facts.html.