SPIDER Veins

Spider Veins
Spider veins (also known as telangiectasias) are dilated or broken blood vessels that lie just beneath the surface of the skin. As their name suggests, the shape and appearance of these veins resemble spider webs. Spider veins are most often found in the thighs and lower legs. However, other health conditions may cause their formation in other parts of the body.
Studies show that around 41 percent of women over the age of 50 develop spider veins. While they are generally harmless, spider veins may also be a sign of underlying vein issues. If you are experiencing other symptoms such as swelling or burning, it may be time to see your doctor or a vein specialist for treatment.
What Are Spider Veins?
Despite their name, spider veins are not actually veins. Instead, they are damaged capillaries, arterioles, or venules underneath your skin. In order to understand what spider veins are, it is important to first learn the names of the different small blood vessels and what they do.
Your vascular system is made of large blood vessels known as veins and arteries, which transport blood, nutrients, and oxygen to your body’s organs and tissues. Your arteries are responsible for carrying oxygen-rich blood from your heart and lungs out to other tissues in your body. Your veins are responsible for bringing oxygen-depleted blood from your tissues back toward your heart and lungs.
Think of your arteries and veins as major highways — from these roads, smaller blood vessels branch off of them out toward your tissues. Arterioles are smaller arteries, and venules are smaller veins. They connect with your capillaries, which are very small blood vessels that act as exchange points for oxygen, nutrients, and waste within your tissues.
Your skin is the largest organ in your body, and it needs plenty of oxygen and nutrients to stay healthy. Some blood vessels that sit under the skin help regulate your body temperature as well. For example, arterioles dilate to help you cool off — they can also constrict to bring blood away from your skin, keeping your body’s core warm.
How Do Spider Veins Form?
Spider veins form when your capillaries, arterioles, or venules underneath your skin become damaged. The walls of these small blood vessels become weakened and lose their ability to expand and contract. Eventually, they dilate too much and become visible. Some people may also have “matted” spider veins or clusters that make a red or pink patch on their skin.
For the most part, spider veins are harmless and are not associated with any troublesome symptoms. However, they may be a sign of underlying vein issues.
Venous Insufficiency
Venous insufficiency occurs when your veins (mainly in your legs) become damaged, typically from increased blood pressure or injury. Your veins have one-way valves in them that ensure blood flows in the correct direction back to your heart. When they are damaged, blood begins flowing backward and pools in your feet, ankles, and legs. The extra fluid increases pressure, eventually leading to swelling and further damage.
Spider veins may be an early sign that your valves are damaged. This may cause blood to flow back into the superficial veins underneath your skin. The extra pressure dilates the smaller blood vessels, eventually making them visible.
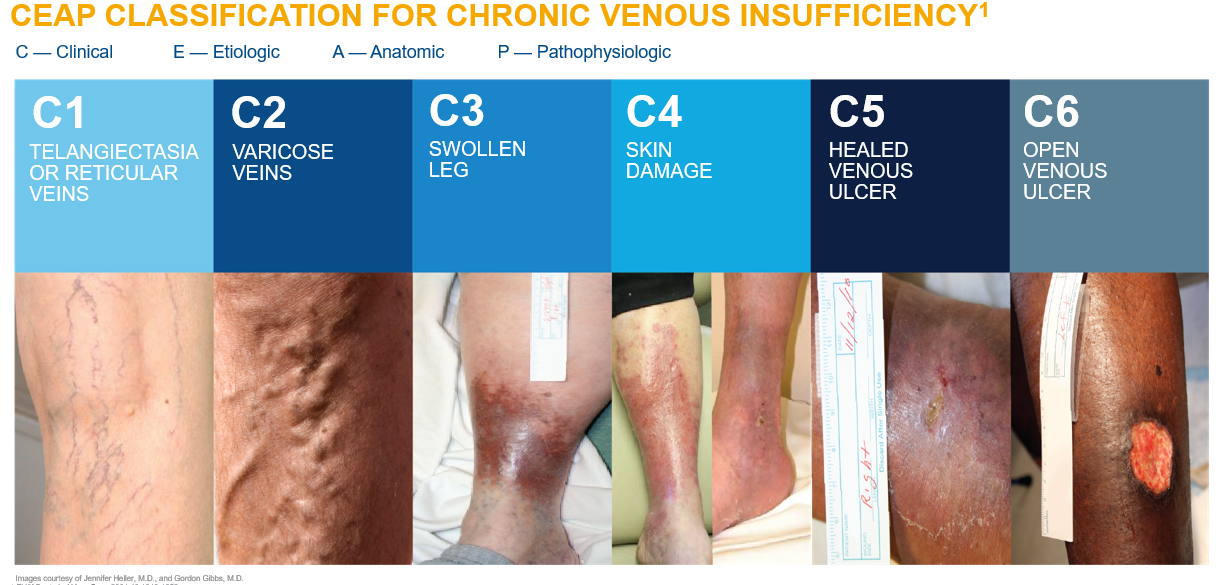
Chronic venous insufficiency (CVI) is a vein disease characterized by swelling, skin damage, and open wounds (ulcers) on the skin. CVI develops slowly over time as a result of faulty valves. The disease is staged using a classification system based on symptoms and vein changes. While spider veins are not considered CVI (which is diagnosed at stage C3), they still may be a sign of potential issues later on.
If you notice any new spider veins, talk to your doctor or book an appointment with a vein specialist. They can help you address any new problem veins before they become worse.
To learn more about venous insufficiency,
read here.
Spider Veins Versus Varicose Veins
Some people may think that spider veins and varicose veins are the same conditions. However, varicose veins are larger damaged veins that are twisted and bulge out from underneath the skin. It is possible for a person to have smaller spider veins near or around larger, dark blue varicose veins. While they are not considered CVI, varicose veins are more severe than spider veins and indicate that you have a form of venous insufficiency.
On the other hand, spider veins tend to be more red or purple in color and turn to white when you press on them. You cannot feel these veins under your skin. Most people seek treatment for cosmetic reasons.
Risk Factors and Causes of Spider Veins
There are several risk factors that increase your chances of developing spider veins. Some of these are in your control, while others are not. Your doctor or vein specialist can help you better understand your specific risks and what steps you can take to prevent new or worsening spider veins.
Family History of Spider Veins
If you have a family history of spider veins, varicose veins, or venous insufficiency, you are more likely to develop these conditions yourself. Studies show that certain genes involved in how the vascular system develops can increase your risk of spider veins and varicose veins. These genes are passed down through family members. It is important to note that just because someone in your family has spider veins, it does not mean that you will develop them.
Sun Exposure
Ultraviolet (UV) light from the sun can damage your skin, but did you know it can also damage your veins? Prolonged sunlight exposure or excessive tanning bed use damages the collagen in your skin and blood vessels, making them stand out. The heat from the sun can also aggravate existing spider veins, causing more dilation and swelling.
Be sure to apply sunscreen often and cover up your legs to avoid new or worsening spider veins. If you have recently had a minimally invasive treatment for a vein issue, your vein specialist will recommend avoiding direct sunlight for a few months to prevent further damage. Some people choose to undergo treatment during the winter to avoid complications from sunlight exposure.
Pregnancy and Hormonal Changes
Research shows that women are more likely to have spider veins than men. This is because female sex hormones — including estrogen and progesterone — fluctuate throughout a woman’s life. These hormones are known to make collagen fibers in your blood vessels relax, causing the blood vessels to relax and dilate. Over time, they lose their elasticity, making it harder for them to return to their original shape and size.
Women who use hormonal birth control such as the pill, patch, intrauterine device (IUD), shot, or vaginal ring are more likely to have damaged vein valves. Estrogen therapy to help treat menopause symptoms can also have the same effects.
The risk of spider veins also increases for pregnant women due to a combination of hormonal changes and added pressure on their blood vessels. During pregnancy, a woman’s blood volume nearly doubles, and this extra fluid can damage the small, delicate blood vessels under the skin. As the baby continues to grow, the uterus puts even more pressure on the leg veins, damaging the valves.
Sitting or Standing for Long Periods of Time
Inactivity for long periods of time throughout the day can lead to spider veins. Your calf muscles act as a “second heart”, squeezing the deep veins in your legs to move blood upward. If you stand or sit for several hours, this pumping action does not happen and blood begins to pool in your feet and legs. Over time, this leads to increased pressure and eventually, spider veins.
Cashiers, teachers, and other professionals who stand in the same place for most of the day tend to develop spider veins. Additionally, office workers who are seated at a desk and those who lead more sedentary lifestyles are at a higher risk.
Smoking and Other Lifestyle Choices
While you cannot control your family history of spider veins, you can make conscious lifestyle choices that affect your vein health. Smoking tobacco constricts your blood vessels, limiting the amount of blood that travels through them. This can increase your blood pressure, damaging your vein valves.
Your body weight also plays a role in developing spider veins. The more weight you carry, the more pressure is put on your leg veins. Over time, this increased pressure weakens the vein walls, causing spider veins.
Autoimmune Diseases and Skin Conditions
An autoimmune disease is caused by your body’s immune system mistaking its own cells and tissues as foreign. Some people with certain autoimmune diseases that attack their connective tissues and skin are at an increased risk of developing spider veins. These include:
- Lupus: attacks your skin, joints, kidneys, and other organs
- Scleroderma: inflammation that causes skin hardening and tightening
- Dermatomyositis: causes red/purple skin rashes and muscle weakness
Other skin conditions associated with spider veins include:
- Rosacea: a condition that causes skin reddening and flushing
- Xeroderma pigmentosa: a condition that makes the skin and tissue covering the eye extremely sensitive to sunlight
- Port-wine stain: a maroon-colored birthmark caused by swollen blood vessels
Symptoms of Spider Veins
For the most part, spider veins are not associated with symptoms. Most people only notice them when they look at their legs. However, some people do develop them as a sign of underlying vein issues. You may notice symptoms if you stand for a long time, such as:
- Cramping
- Burning
- Pain
- Itching
- Muscle fatigue
Talk to your doctor or a vein specialist if you also have signs of
varicose veins, including:
- Swelling in your ankles or legs
- Feelings of fullness or heaviness in your feet or legs
- Aching pain in your legs
- Open sores on your legs, known as venous stasis ulcers
- Discolored skin around bulging veins
- Leg cramping at night (known as nocturnal leg cramps)
To learn more about varicose veins,
read here.
How Are Spider Veins Diagnosed and Treated?
Your doctor or vein specialist can diagnose spider veins simply by looking at the appearance of your legs. They will note where the spider veins are and if you have any varicose veins near them as well. If you are experiencing any uncomfortable symptoms you think may be due to your spider veins, be sure to bring them up during your appointment.
A vein specialist who is specially trained in treating vein diseases will select the best treatment option for you. The best therapies not only clear the appearance of spider veins, but also combat the underlying cause. Two of the most commonly used spider vein treatments that are safe and provide long-lasting results are
sclerotherapy and laser therapy.
Most vein specialists use minimally invasive techniques to treat spider veins. These procedures have little to no downtime for healing, getting you back on your feet sooner.
Sclerotherapy
Sclerotherapy is a preferred technique for treating spider veins and any associated small varicose veins. The vein specialist will inject a salt or chemical solution (known as a sclerosing agent) through the needle. This solution causes the vein to collapse in on itself, blocking off blood flow. On average, the procedure takes 30 minutes.
Afterward, your vein specialist may have you wear compression stockings or special garments that apply pressure to your feet and legs. They help encourage blood to move upward toward your heart. Keeping your legs elevated above your heart can also harness the power of gravity to stop blood pooling.
Many people see results after sclerotherapy within a few weeks of treatment. Depending on how severe your spider veins are, you may need more than one session with your vein specialist. They will discuss your specific treatment plan with you during your consultation.
To learn more about sclerotherapy,
read here.
Laser Therapy
Unlike sclerotherapy, laser therapy is a non-invasive technique that uses light energy and heat to clear away spider veins. During this procedure, the vein specialist will use a specialized laser and place it directly over the spider veins. It creates short, intense pulses of light — some people see improvements immediately, while it may take multiple sessions for others. If you also have varicose veins, it may take up to three months for them to disappear.
Your vein specialist will likely have you wear compression stockings after the procedure. You should also protect the treated skin from the sun for around one month to prevent skin darkening and new spider veins.
Preventing and Managing Spider Veins
After your spider vein treatment, there are extra steps you can take to help stop their return. Your vein specialist will likely recommend some lifestyle changes, such as:
- Wearing sunscreen with a sun protection factor (SPF) of at least 30 — not only does this help protect your skin from damage, but it also protects your veins
- Continue wearing your compression stockings, especially if you stand for several hours throughout the day
- Elevate your legs after a long day of sitting or standing to encourage blood flow back toward your heart — this can also help reduce any swelling you may have
- Get more exercise to work your calf muscles and keep blood pumping throughout your entire body
- Stand up at regular intervals throughout the day if you sit at a desk — you can reflex your calf muscles or foot and ankle while sitting to mimic the pumping action of walking
- Maintain a healthy weight to help alleviate pressure off of your leg veins
- Limit your time in direct sunlight, saunas, or hot tubs, as heat can dilate and damage blood vessels in some people
- Try to avoid wearing high heels, tight socks, and tight clothing, as these can interfere with the normal blood flow in your feet and legs
Complications from Spider Veins
Sometimes, if left untreated, spider veins may progress to CVI and increase your risk of other health problems. CVI is diagnosed when you have spider veins, varicose veins, and leg swelling. In more severe cases, you may also have skin discoloration, thickening, or texture changes, and ulcers. It is important to address problem veins sooner rather than later to avoid lasting damage to your legs.
CVI also increases your risk of cellulitis, a skin infection that occurs when bacteria get into ulcers. Signs of cellulitis include swollen, red, painful skin that feels warm to the touch. Your skin may also appear dimpled or pitted.
Frequently Asked Questions (FAQ)

DR. AMIT POONIA M.D.
Your New Jersey Vein Specialist
Dr. Poonia is double board-certified in interventional pain management and anesthesiology.
Dr. Poonia’s philosophy is based on teamwork, cooperation, and collaboration among his patients’ treatment teams. He believes that healthcare providers work
best when they work together to accurately diagnose a patient’s problem, find effective treatments, and provide maximum rehabilitation and quality of life improvements.
Dr. Poonia customizes his treatment plans based on each patient’s unique characteristics. He employs the latest minimally-invasive technologies to enhance comfort during treatment and to speed recovery.
References
- Arterioles. June 25, 2022. Accessed January 26, 2023. https://my.clevelandclinic.org/health/body/23377-arterioles
- Bernstein EF, Kornbluth S, Brown DB, Black J. Treatment of spider veins using a 10 millisecond pulse-duration frequency-doubled neodymium YAG laser. Dermatol Surg. 1999;25(4):316-320. doi:10.1046/j.1524-4725.1999.08253.
- Capillaries. Cleveland Clinic. October 5, 2021. Accessed January 26, 2023. https://my.clevelandclinic.org/health/body/21988-capillaries
- Cellulitis. Centers for Disease Control and Prevention. June 27, 2022. Accessed January 26, 2023. https://www.cdc.gov/groupastrep/diseases-public/Cellulitis.html
- Chronic Venous Insufficiency. Cleveland Clinic. July 17, 2022. Accessed January 26, 2023. https://my.clevelandclinic.org/health/diseases/16872-chronic-venous-insufficiency-cvi.
- Leg Veins: Why They Appear and How Dermatologists Treat Them. American Academy of Dermatology Association. Accessed January 26, 2023. https://www.aad.org/public/cosmetic/younger-looking/how-dermatologists-treat-leg-veins
- Mujadzic M, Ritter EF, Given KS. A Novel Approach for the Treatment of Spider Veins. Aesthetic Surg J. 2015;35(7):NP221-229. doi:10.1093/asj/sjv004
- Nijsten T and van den Bos RR, et al. Minimally invasive techniques in the treatment of saphenous varicose veins. J Am Acad Dermatol. 2009;60:110-119. doi:10.1016/j.jaad.2008.07.046.
- Sclerotherapy. Cleveland Clinic. June 12, 2022. Accessed January 26, 2023. https://my.clevelandclinic.org/health/treatments/6763-sclerotherapy
- Smith PC. Management of reticular veins and telangiectases. Phlebology. 2015;30(2 Suppl):46-52. doi:10.1177/0268355515592770.
- Spider Veins. Cleveland Clinic. December 29, 2023. Accessed January 26, 2023. https://my.clevelandclinic.org/health/diseases/24567-spider-veins
- Telangiectasia. MedlinePlus. June 19, 2021. Accessed January 26, 2023. https://medlineplus.gov/ency/article/003284.htm
- Telangiectasia and Autoimmune Disease. Hospital for Special Surgery. July 19, 2019. Accessed January 26, 2023. https://www.hss.edu/conditions_telangiectasia-and-autoimmune-disease.asp
- Varicose Veins and Spider Veins. Office on Women’s Health. February 15, 2021. Accessed January 26, 2023. https://www.womenshealth.gov/a-z-topics/varicose-veins-and-spider-veins
- Worthington-Kirsch RL. Injection sclerotherapy. Semin Intervent Radiol. 2005;22(3):209-217. doi:10.1055/s-2005-921954.